by O’Neil Pyke, MD
Healthcare in the US is once again in the midst of yet another massive overhaul. And at the center of it, we find the specialty of Hospital Medicine (HM). Still in its infancy, HM has been tasked with the duty of championing the healthcare changes within the walls of the hospital; and in many cases, beyond.
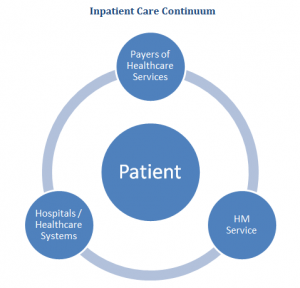
Led by CMS, the payers of healthcare services are purposefully moving away from a quantity based payment system to now embrace patient safety and quality as the key endpoints. Essentially, the current healthcare environment is demanding more accountability and higher quality of care, with an overarching goal of cutting cost. Daunting indeed, but these are the marching orders for hospital executives across the US. It is therefore crucial that we pause to better understand the current imperatives of the modern hospital and hospital executives to assure proper alignment. In other words, the HM service must present itself as a visible partner in the care of patients in the hospitals to complete the Inpatient Care Continuum (ICC).
In many ways, HM was borne out of this emerging need to improve quality of care and outcomes, not to mention the disastrous financial implications of failure. One of the key questions for hospitals and healthcare executives (and therefore HM services) is: what constitutes success and how will failure reveal itself? Before answering those questions, let’s review a few definitions. HM, as defined by the Society of Hospital Medicine (SHM), is defined as:
“A medical specialty dedicated to the delivery of comprehensive medical care to hospitalized patients.”
Further, SHM defines a hospitalist as:
“A physician who specializes in the practice of hospital medicine. Following medical school, hospitalists typically undergo residency training in general internal medicine, general pediatrics or family practice, but may also receive training in other medical disciplines.”
In today’s healthcare landscape, a hospitalist must be more, do more and accomplish all this with even fewer resources compared to their predecessors. For true sustainability, alignment and success of HM, I submit the following as a more accurate definition of the hospitalist:
“A generalist (Internal Medicine or Family Practice Physician or Advanced Practice Provider) who merges a strong clinical skill set with a superior understanding of the operational components necessary to implement systems improvement and efficient coordination of patient care.”
Going forward, Hospitalist programs will not be afforded the option of just “getting by” with staffing the service. Full alignment will be demanded (as it should be). As the payers of healthcare services, led by CMS, hold the hospitals accountable, the hospitals will in turn hold the providers accountable. Practice Management organizations, MUST respond loud and clear to this healthcare challenge. Client hospitals are simply seeking solutions that have not been afforded to them by their current staff and/or structure.
The key here is partnership: meeting the client hospitals where they underperform and helping to guide them toward innovative solutions. The success of HM services will hinge on proactive examination of the institution(s) and delivering patient-centered, cost effective and evidence-based care. Again, this is a daunting task, but with the correct deployment of resources, it is attainable.

 Search
Search

 Search |
Search |