
Featuring commentary from Tye Murray, RN, Nurse Liaison and Elizabeth James, MD, Regional Medical Director
Every emergency department is different. That seems like a no brainer—but in an age of metrics, where hospitals are categorized by trauma level and lumped together based on payor mix, annual visits, and a host of other numbers, it’s important to remember that ED management isn’t one-size-fits-all. When it comes to patient flow, every ED really is a snowflake. Every ED deals with different volumes, staffing levels, physician quality, and community factors, and the list goes on.
Management techniques and strategies must be custom fit to meet each ED’s needs, especially when it comes to the intricate and demanding process of patient flow. Enter our resident patient flow experts, Tye Murray, RN and Elizabeth James, MD. After talking to them, as well as a few of our site medical directors, I was able to get an idea of the basics of patient flow and just how challenging it is. I’ve pulled together their thoughts into a few key ideas on what it takes to sustain successful patient flow.
1. The Administrator/CEO has to be involved in the patient flow discussion
Tye and Dr. James could not stress this enough. In their experience, when the CEO is interested in and supportive of patient flow improvement, patient flow improves. When he or she is not, patient flow can’t improve.
Tye: “We can hand out the tools, but at the end of the day, we’re not their boss, and we can’t hold them accountable for the things they’re supposed to do.
Dr. James: “If the administrators are present, they are able to understand the processes of all these departments and how they affect each other. It gives them a big picture, and helps them more rapidly and correctly identify solutions to problems. If we don’t have his or her support, engagement, and commitment, we will not succeed at the task that the hospital has hired us to do.”
2. As always, communication is key
Hospitals of any size have communication challenges. Without open communication, silos form and patient care suffers.
Tye: “When there are so many providers, sometimes it’s hard to know the workflow of everyone else… Having a really good charge nurse is the key to any ED patient flow. They know what’s going on with every provider and every patient, and they’re able to direct flow. When there is a mismatch between patient demand and ED capacity to take care of patients, it leads to poor patient flow and departmental crowding. And that’s when it starts to be associated with quality of care delivered, and ultimately, poor patient outcomes.”
Dr. James: “If the floors are not involved with the ED’s patient flow and discharging patients before noon, or if there are silos between Hospitalists, nursing staff and ED physicians, then there is a huge bottleneck.”
3. Every department needs to be involved, from the C-Suite to Housekeeping
When Keystone steps into a new client location, often the first initiative we establish is the Monthly Patient Flow Meeting (MPFM). This is a meeting that takes place once a month, and ideally involves at least one stakeholder from every single department. This includes Keystone team members, Nursing, C-Suite, IT, EMS, Case Management, and yes, even Housekeeping.
Tye: “We are there for way more than just patient flow. [The MPFM] gives us a global picture to review key processes and metrics. That could be anything from case management to documentation processing.”
Dr. James: “It’s an opportunity to break down silos. We look at what other departments are doing and how that affects our flow, and vice versa.”
4. Action items keep everyone accountable
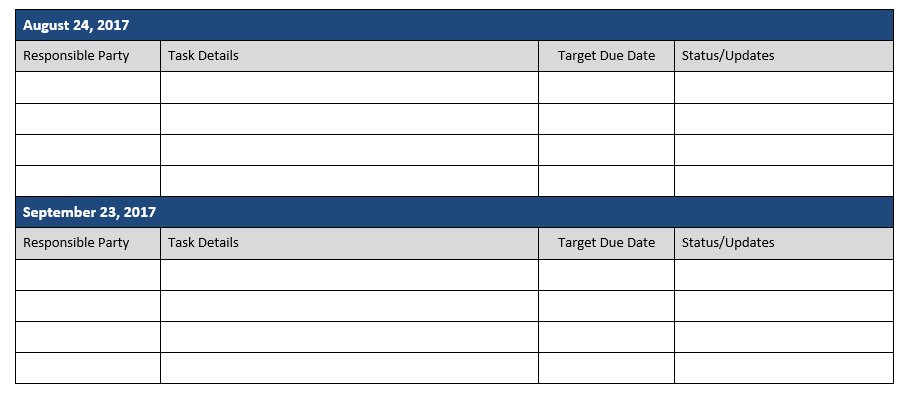
At each MPFM, team members are given action items and are held accountable for updating the team on the progress of the items they own. This eliminates the problem of people forgetting what they were supposed to do, and it helps teams keep track of the progress they’ve made (or haven’t made).
Tye: “What I do is I just keep sending the action items out—I send them out as soon as possible after the meeting, and then two weeks after the meeting, and then a week before the meeting, so that it’s not something that is forgotten about. Sometimes things take longer than we initially think, but if you know that somebody is working on them, or that certain things that have to happen before other things can happen, then that’s another story.
Dr. James: “I think if you write [action items] down, it’s obvious to us when we look at those action items who has made progress and who has not. We have implemented it, and we have watched it really work. That is our way for us as clinicians to connect with [administration] on a business level. You have to have accountability.”
Now that I’ve managed to simplify patient flow into four basic ideas, it’s time for a disclaimer: patient flow is not that simple. In Tye’s words, “It’s a whole process.” But implementing some of the strategies mentioned here can transform the big picture, and that can change the bottom line.
Have any questions about this article? Reach us @KeystoneHCMGMT!

 Search
Search

 Search |
Search | 



